Stem Cell Therapy for PPMS: Treatments, Research & Benefits

10,000+ subscribers
Join our newsletter to learn more about stem cell therapy and the science behind it.
Primary progressive multiple sclerosis (PPMS) is a debilitating form of MS that affects approximately 10-15% of all people diagnosed with the disease. Unlike relapsing-remitting MS (RRMS) and secondary progressive multiple sclerosis (SPMS), which are characterized by periods of relapse and remission, primary progressive MS (PPMS) follows a more constant progression, with symptoms worsening over time. The immune system plays a significant role in the development of PPMS, causing inflammation and damage to nerve fibers in the central nervous system.
Conventional disease-modifying therapies have limited effectiveness in treating PPMS, leading researchers and the multiple sclerosis association to explore alternative treatment options. One promising avenue is stem cell therapy, which has shown potential in improving neurologic function, reducing inflammation, and slowing down MS progression.
While PPMS patients tend to experience fewer inflammatory cells and lesions compared to those with relapsing forms of MS, they often require more assistance in managing their symptoms and daily activities. As stem cell therapy continues to gain traction as a potential treatment for PPMS, it is crucial to remain vigilant in understanding its benefits, risks, and long-term effects on patients living with this challenging disease.
{{protocol="/styling"}}
Understanding PPMS
Primary Progressive Multiple Sclerosis (PPMS) is a rare form of multiple sclerosis (MS) that affects the central nervous system, including the brain and spinal cord. Unlike relapsing-remitting multiple sclerosis (RRMS), PPMS is characterized by a steady progression of neurological function without relapses or remissions. This relentless decline in function can significantly impact a person's everyday activities and quality of life.
Diagnosing PPMS
Diagnosing PPMS can be challenging, as there is no single diagnostic test. Instead, healthcare providers use a combination of clinical observations, medical history, and diagnostic tests such as MRI scans and lumbar punctures. An accurate diagnosis is crucial for determining the best course of treatment and managing symptoms effectively. Doctors must rely on a combination of patient history, clinical examination, MRI scans, lumbar puncture (spinal tap), and analysis of spinal fluid to determine the presence of the disease. Common symptoms of primary progressive MS include muscle spasms, pain, disability, and sexual problems, all of which can significantly affect a person's quality of life.
Treating PPMS
There is no cure for PPMS, but various disease-modifying therapies (DMTs) and medications can help manage symptoms and slow down disease progression. However, the available treatment options for PPMS are limited compared to those for other forms of MS, such as RRMS.

Stem Cell Therapy for PPMS
Stem cell therapy, specifically the use of mesenchymal stem cells (MSCs), is a novel approach to treating primary progressive MS (PPMS). This innovative therapy aims to improve disease state by reducing inflammation, regulating immune cells, and potentially promoting tissue repair. The immunomodulatory, tissue-protective, and repair-promoting properties of MSCs make them an attractive therapeutic option for multiple sclerosis and other conditions characterized by inflammation or tissue injury.
{{protocol="/styling"}}
Benefits of Stem Cell Therapy in PPMS Patients
Patients undergoing stem cell therapy for PPMS may experience increased energy, flexibility, strength, mobility, and control of essential functions. Recent data suggests that intravenously administered MSCs might even have the ability to halt disease progression for an extended period.
The Role of Mesenchymal Stem Cells in Treating MS
MSC therapy offers a promising alternative to traditional MS treatments. Research has shown that stem cells have the potential to repair the myelin sheath, a protective covering around nerve fibers in the central nervous system that becomes damaged in MS. Furthermore, MSCs can modulate the immune response, which is thought to be involved in MS development.
The Potential of MSCs to Protect and Repair Nerve Cells
A study published in Stem Cell Research & Therapy in 2019 indicates that MSCs may protect nerve cells from damage by reducing inflammation and oxidative stress while promoting remyelination. However, it is crucial to note that stem cell therapy for MS is still in the early stages of research and development, and further studies are needed to determine its long-term efficacy.
Expanded cord tissue-derived umbilical cord cells have shown potential for treating MS more effectively, with studies conducted on both secondary progressive MS and relapsing-remitting MS. Administered MSCs can help regulate the immune system and prevent further myelin degradation, making them an attractive therapy for MS and other conditions characterized by inflammation or tissue injury. Some patients have even reported significant improvements in symptoms such as peripheral neuropathy.
Advantages of Stem Cell Therapy for Multiple Sclerosis
The advantages of stem cell therapy for MS include the ability of MSCs to help regulate the immune system, repair damaged myelin sheath or neurons, and provide a high number of mesenchymal cells from umbilical cord tissue. Furthermore, stem cells have potent anti-inflammatory properties, allowing for tissue repair and regeneration. IV stem cell therapy is non-invasive and does not require downtime, potentially reducing debilitating MS symptoms and stabilizing the condition or extending periods of remission.
The success rate of MSC therapy for multiple sclerosis is still under investigation, with limited studies reporting primarily positive results. Some studies on relapsing forms of MS have reported improvements in symptoms and reduced inflammation following MSC therapy. However, larger studies and more research are necessary to confirm the safety and efficacy of MSC therapy for MS.

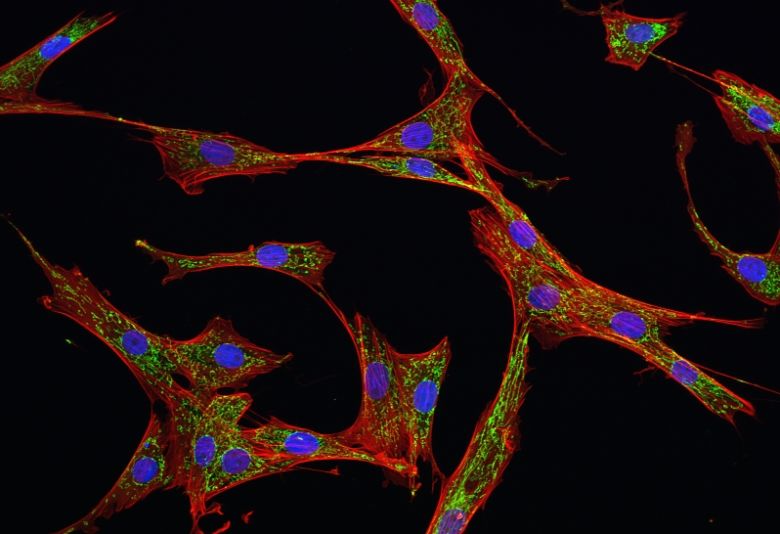
The Science Behind Stem Cells
Stem cells are unique cells that have the potential to develop into many different cell types, including nerve cells. In recent years, stem cell therapy has emerged as a promising treatment for various neurological disorders, including MS.
Mesenchymal Stem Cells
Mesenchymal stem cells (MSCs) are a type of stem cell that can differentiate into various cell types, including nerve cells. MSCs also have anti-inflammatory and immunomodulatory properties, making them a potential treatment for PPMS. Learn more about mesenchymal stem cells here.
Stem Cell Therapy Success Rate
Research on the success rate of stem cell therapy in multiple sclerosis is still ongoing. However, early studies have shown promising results, with some patients experiencing reduced inflammation and improved neurological function. Find more information about the success rate of stem cell therapy in MS here.
The Process of Stem Cell Therapy for PPMS
- Before undergoing stem cell therapy for PPMS, patients must undergo a thorough evaluation by a healthcare provider. This evaluation will help determine the suitability of stem cell therapy for the patient and establish a personalized treatment plan.
- The stem cell therapy process involves the extraction of stem cells, either from the patient's own body or from a donor. The cells are then processed and expanded in a laboratory to ensure they meet the required criteria for treatment. Once the stem cells are prepared, they are administered to the patient through an intravenous infusion or injection into the affected area.
- Following stem cell therapy, patients are closely monitored by their healthcare provider to track their progress and assess the effectiveness of the treatment. Some patients may require additional treatments or follow-up care to ensure optimal results.
{{data="/styling"}}
Managing PPMS
Managing Multiple Sclerosis (MS) involves a combination of medical treatments, lifestyle adjustments, and support networks to improve the patient's quality of life, alleviate symptoms, and slow disease progression.
Lifestyle Changes
Adopting a healthy lifestyle can help improve overall well-being and slow down the progression of PPMS. This includes maintaining a balanced diet, getting regular exercise, and prioritizing sleep. Find out how to increase natural stem cell production with a healthy diet here.
Exercise and Physical Therapy
Regular exercise and physical therapy can help maintain muscle strength, flexibility, and balance, which are crucial for people with PPMS. Exercise may also improve mood and overall quality of life. Learn how exercise can help PPMS here.
Occupational Therapy
Occupational therapy can help people with PPMS adapt to their changing abilities and maintain their independence in daily activities. This may include learning new techniques for performing tasks or using adaptive equipment.
Emotional and Mental Health Support
Living with PPMS can be challenging, and it is essential to address the emotional and mental health aspects of the disease. Support from friends, family, and healthcare professionals can help individuals cope with the challenges of PPMS.
Comparing PPMS to RRMS
Primary progressive multiple sclerosis (PPMS) and relapsing-remitting multiple sclerosis (RRMS) are two distinct forms of MS, differing in their progression, symptoms, and treatment approaches.
PPMS is characterized by a steady worsening of neurological function without distinct relapses or periods of remission. Symptoms gradually worsen over time, often leading to increased disability. PPMS is less common, affecting approximately 10-15% of people with MS. There are limited treatment options for PPMS, and it can be more challenging to manage compared to RRMS.
RRMS, on the other hand, is the most common form of MS, affecting around 85% of people with the disease. It is characterized by clearly defined relapses (flare-ups) followed by periods of partial or complete recovery (remission). During remission, symptoms may disappear or stabilize, with little to no disease progression. RRMS generally has a wider range of available treatments, including disease-modifying therapies, which can help manage symptoms and reduce the frequency of relapses.
Key Differences
PPMS and RRMS are both forms of MS but differ in their progression and symptoms. RRMS is characterized by periods of relapse and remission, while PPMS follows a steady progression without relapses. The treatment options for PPMS are also more limited compared to RRMS.
Severity of PPMS vs. RRMS
PPMS is generally considered more severe than RRMS due to its progressive nature and lack of remissions. However, the severity of the disease varies among individuals, and some people with PPMS may have a milder course.
{{apply2="/styling"}}
Conclusion
In conclusion, primary progressive MS (PPMS) is a complex and challenging form of multiple sclerosis that affects a person's life significantly. Unlike relapsing-remitting MS and secondary progressive MS, PPMS tends to follow a steady course of worsening symptoms without periods of remission. Diagnosing PPMS can be a difficult process, as doctors must rely on various diagnostic tools, such as MRI scans, to identify the disease based on specific criteria.
Individuals with PPMS may not experience relapses like those with other forms of MS, but they often contend with progressively worsening symptoms that can impact their daily lives. As a result, doctors and patients alike are continually searching for more effective treatment options. Disease-modifying therapy, while beneficial for some, has limited effectiveness in treating PPMS.
Stem cell therapy has emerged as a promising alternative treatment for PPMS, offering hope to those who struggle with the disease's relentless progression. As research continues to advance our understanding of PPMS and its underlying mechanisms, it is crucial to explore and develop new treatments that can improve the quality of life for affected individuals. The journey towards a better understanding of PPMS and more effective treatment options is ongoing, and the experiences of each person living with this condition will help shape the future of PPMS care and management.
Frequently Asked Questions
What is the best treatment for PPMS?
There is no one-size-fits-all treatment for PPMS, as the best approach depends on the individual's specific symptoms and disease progression. Current treatment options include disease-modifying therapies, medications to manage symptoms, and stem cell therapy.
Can stem cells reverse MS damage?
Stem cell therapy has shown promise in reducing inflammation and promoting the repair of damaged nerve cells in MS. However, more research is needed to determine the full extent of stem cell therapy's potential to reverse MS damage.
Can you reverse PPMS?
There is currently no cure for PPMS, and reversing the disease is not possible. However, treatments like stem cell therapy may help slow down disease progression and improve overall quality of life for individuals with PPMS.
What is the average age of death for PPMS?
The life expectancy for individuals with PPMS varies depending on factors such as the severity of the disease and the effectiveness of treatments. While PPMS can shorten life expectancy, many people with the condition can live relatively normal lives with proper management and care.
Does exercise help PPMS?
Yes, exercise can help individuals with PPMS maintain muscle strength, flexibility, and balance. Regular physical activity may also improve mood and overall quality of life. It is essential to work with a healthcare professional to develop an appropriate exercise plan tailored to individual needs and abilities.
.webp)